Introduction
Your parrot sneezes. Cute, right? You smile, maybe even mimic it back. But what if that sneeze can put you in the hospital? It's hard to picture danger in a bird so vibrant and charming. However, hidden in its feathers and dried droppings may be a microscopic hitchhiker that you'll never notice—Chlamydia psittaci, the bacterium behind a disease called psittacosis.
This isn't just a rare freak occurrence. It's a real disease with a history of shutting down pet stores, halting bird imports, and causing mass hysteria. They call it "parrot fever," but its reach and breadth go beyond parrots. In this article, we’ll explore what psittacosis is, how it spreads, survives, and hides, revealing why a simple sneeze from your bird can be more dangerous than it looks.

Psittacosis and Its Many Bird Hosts
Chlamydia psittaci is not your average germ. This gram-negative, obligate intracellular bacterium lives as a parasite in host cells. They use host machinery to reproduce before infecting the next host.
The name "psittacosis" comes from the Greek word psittakos, meaning "parrot." This name was coined in the late 19th century when imported parrots were the most notorious carriers of the disease. However, the name "parrot fever" can be misleading. Scientists have now identified over 467 bird species that can harbour C. psittaci, including pigeons, poultry, and many wild birds.
History bears witness to how dangerous this tiny bacterium can be. In 1929–1930, a psittacosis outbreak in the United States and Europe whipped up public panic. Media reports at the time amplified the danger, leading the public to believe the epidemic was larger than it actually was. They also shut down pet shops and prohibited bird imports. The outbreak prompted significant changes in regulations on animal trade and disease reporting.

Psittacosis Transmission and Pathophysiology
The story of Chlamydia psittaci often begins unnoticed. It could be the dust cloud when you're cleaning a birdcage, a parrot's sneeze. This bacterium is found on dried droppings, feather dust, or respiratory secretions. They drift unnoticed into the air you breathe. Inhalation is by far the most common way to become infected. Additionally, a slight peck with a beak or a kiss on a bird's head can spread the infection. Even contact with an infected egg can also spread the infection.
The tenacity of the bacterium contributes to its threat. C. psittaci is able to survive for weeks outside a host. When inhaled, the pathogen enters its resilient "elementary body" form, which is a microscopic capsule built for survival. It attaches to cells deep in the lungs and inserts itself within. They now morph into their "reticulate body" form, which is built for replication. The cell ultimately bursts, releasing new infectious agents into the bloodstream to seek out new targets.
In response, the immune system reacts like an alerted city guard. They flood the lungs with inflammatory cells in an attempt to trap the invader. This inflammation slows down the spread of infection but also damages delicate lung tissues. Meanwhile, some of the bacteria outsmart the defences. They travel through the bloodstream to infect other organs. In severe cases, C. psittaci can spread to the heart, liver, or even the brain.

Psittacosis Symptoms, Severity, and Complications
Psittacosis doesn't announce itself with anything unusual at the beginning. After a 5-to-14-day incubation period, it typically presents with vague and flu-like symptoms. These symptoms include fever, chills, pounding headache, sore muscles, diarrhoea, or a faint rash known as Horder's spots. Early symptoms can be easily mistaken for a seasonal infection, which is why many cases aren't detected in the early stages.
If the infection continues, it tends to move towards the lungs, where it causes atypical pneumonia. The cough is typically dry, with shortness of breath and crushing fatigue that can render even minor tasks exhausting. This respiratory stage can persist for weeks without treatment, grinding the body down.
However, Chlamydia psittaci is more than just a lung infiltrator. In more severe infections, the bacteria disseminate to other parts of the body through the bloodstream. They cause inflammation of the heart (myocarditis or endocarditis), liver (hepatitis), or brain (encephalitis). In very severe instances, acute respiratory distress syndrome (ARDS) can result.

Diagnosis of Psittacosis and Why It's Hard
Psittacosis is hard to diagnose since it lacks a clear calling card. Its symptoms, such as cough, fever, and fatigue, are virtually indistinguishable from influenza, COVID-19, or any other respiratory infection. Without any historical clue, it can be mistaken for something far more trivial. In most cases, the eureka moment comes when a clinician asks, "Do you keep birds? That single question can change the course of the investigation entirely.
Once suspected, modern devices can nail down the culprit. PCR testing is the gold standard because it's fast, precise, and able to detect Chlamydia psittaci DNA from respiratory samples. Serology testing, which looks for rising antibody levels, provides evidence of a recent infection. Metagenomic next-generation sequencing (mNGS) has the potential to reveal even minute quantities of bacterial genetic material. They are incredibly useful when other tests are inconclusive. Culture remains possible but is rarely attempted outside high-containment BSL-3 labs due to safety reasons. Because psittacosis mimics so many different diseases, timing is everything.
Respiratory illnesses from birds can look strikingly similar, making them tricky to tell apart. Curious about how psittacosis stacks up against bird flu? Check out our Bird Flu Complete Guide for the key differences and latest updates.
Treatment, Recovery, and Prevention
The treatment of psittacosis typically involves doxycycline or another tetracycline-class antibiotic for 7–14 days. These drugs prevent Chlamydia psittaci from replicating in host cells. In pregnant women or individuals allergic to tetracycline, azithromycin or erythromycin is a good alternative. The beta-lactam antibiotics penicillin and amoxicillin are not effective. This is because the bacterium resides inside host cells, beyond the reach of these drugs.
Most patients, if treated early, will begin to get better within 48 hours. However, stopping antibiotics can lead to the persistence of bacteria. Prevention involves minimizing contact with infectious bird materials. It is advisable to wear gloves and masks when cleaning cages. Also, quarantine new or sick birds before introducing them to others. Routine veterinary visits can identify infection early in bird flocks.

Photo by Darina Belonogova on Pexels
For people in close contact with birds, such as breeders and zoo workers, good hygiene and protective clothing are needed. Additionally, familiarity with symptoms of psittacosis is the best protection. With early treatment and simple prevention, this potentially fatal disease is both treatable and preventable.
Bird-borne diseases reach humans in surprising ways, from dust and droppings to direct contact. Curious about how avian influenza makes that leap? Explore our article on How Bird Flu Spreads to Humans.

Cultural, Historical, and Odd Facts
Psittacosis has a fascinating history as well. In the 1930s, a devastating outbreak of pneumonia wrecked the United States. The origin of the disease was unknown; it was later linked to South American Parrots that were imported into the country. This outbreak led to nationwide panic, strict bird quarantines, and new laws governing importation.
During the Cold War era, Chlamydia psittaci even caught the attention of military researchers. They were the focus of biological weapon research due to their capacity to cause severe respiratory illness. However, there was no indication that it was ever used as a weapon.
One of the most well-publicized cases was that of Lena Rose Pepperdine. She was a pet shop worker whose illness made national headlines. Her story brought awareness to the dangers of working with birds. While transmission is almost always bird-to-human, limited human-to-human transmission has been documented, typically in hospital settings.

Why This Minuscule Bacterium Still Matters
Psittacosis is not just a pet bird problem. Wild and migratory birds also harbor Chlamydia psittaci, quietly moving between continents. As the flocks meet up at shared feeding grounds or stopover wetlands, they may seed the bacterium into entire new regions, occasionally sparking outbreaks far from the source.
Environmental stressors add to the problem. Habitat loss forces birds into close quarters. Also, climate change alters migration routes, bringing bird species whose paths would never naturally meet. When you add pollution and poor nutrition, you've got a perfect storm for increased bacteria shedding.
Global reporting and surveillance are coordinated by the World Organisation for Animal Health (WOAH, formerly OIE) to prevent any outbreaks. Habitats are preserved, and illegal bird trade is combated by BirdLife International. Also, the CDC and FAO promote a One Health approach. This model recognizes that wildlife, livestock, and human health are closely interconnected. So, what happens to one happens to all.

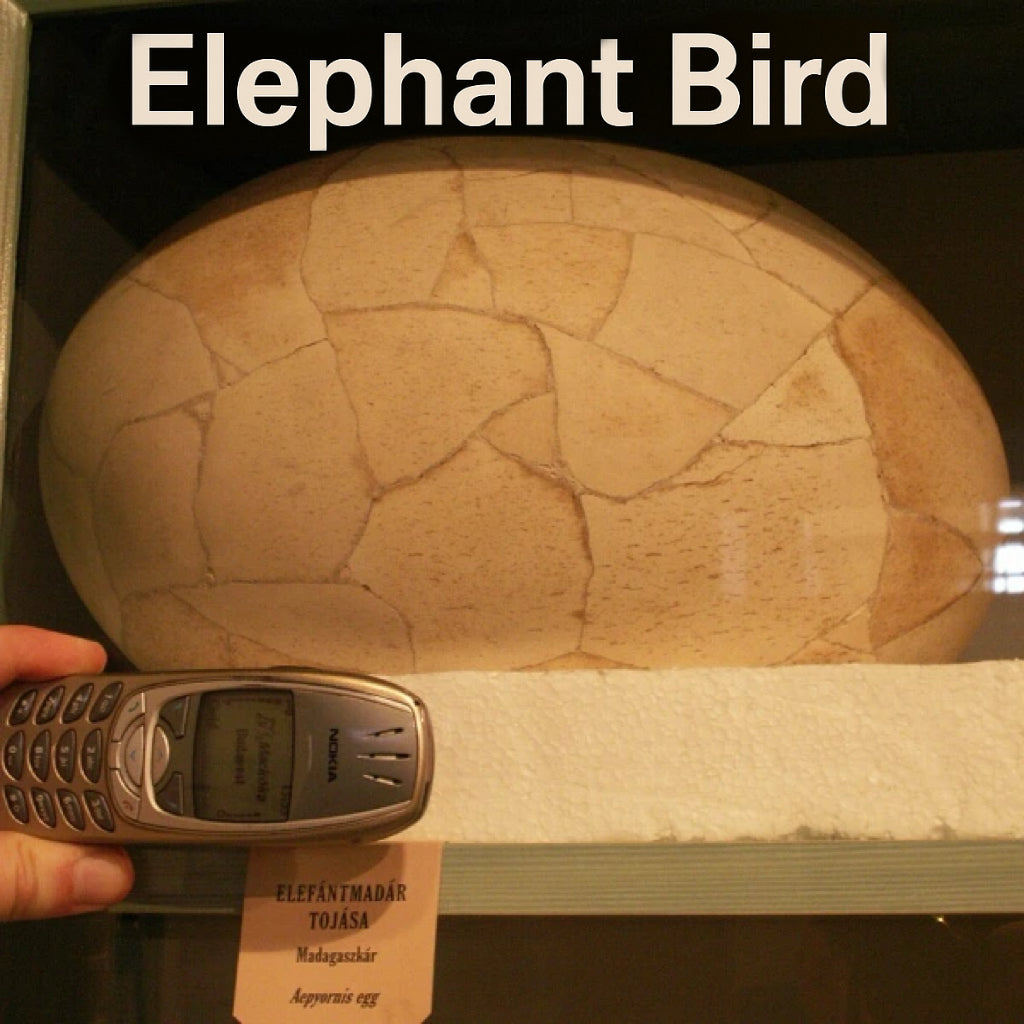
An immature little blue heron with psittacosis
By unknown, via Wikimedia Commons, Public Domain.
Conclusion
Birds bring colour, song, and personality to our lives. But caring for them takes more than just food and love. It involves being aware of the potential risks they may carry. By being clean and responsible bird owners, we are protecting ourselves as well as our pets.

FAQs About Psittacosis
Can I get psittacosis from my bird if it seems healthy?
Yes. Infected birds usually show no signs, but they still shed Chlamydia psittaci in droppings, nasal discharge, and feather dust. Overcrowding, stress, or poor diet can cause more extensive shedding even in seemingly healthy birds.
How common is Psittacosis today?
In the United States, there are fewer than 10 cases reported annually. However, underdiagnosis is likely because of flu-like or pneumonia-like symptoms.
Is Psittacosis life-threatening?
Yes, though deaths are rare (less than 1% with early antibiotic treatment). Delayed or missed diagnosis increases the danger of severe complications like myocarditis, hepatitis, and respiratory failure.
What are the symptoms of psittacosis?
Psittacosis symptoms in humans are often flu-like, including fever, chills, headache, muscle aches, and a dry cough. The illness can range from mild to severe, with a common complication being pneumonia, which may require hospitalization. Symptoms typically begin 5 to 14 days after exposure to the bacteria, usually from infected birds, and can be treated with antibiotics.
Is psittacosis the same as chlamydia?
No, psittacosis is caused by a different bacterial species than the one that causes chlamydia in humans.
How is psittacosis transmitted to humans?
Psittacosis is transmitted to humans primarily by inhaling aerosolized particles from infected birds, such as dried feces, respiratory secretions, and feather dust. Direct contact with infected birds, including a peck or touch, and inhaling contaminated dust can cause infection. Individuals at higher risk include pet bird owners, veterinarians, and poultry workers. Human-to-human transmission is rare.
Can psittacosis be cured?
Yes, psittacosis is generally curable with antibiotics. Most people with psittacosis recover fully after taking a course of antibiotics, such as doxycycline or other tetracyclines. While the illness can be severe in some cases, especially without treatment, prompt antibiotic treatment significantly increases the chances of a quick recovery.


Leave a comment
All comments are moderated before being published.
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.